
Jump to section
Osteoporosis is a global health epidemic, coming in second to cardiovascular disease as a global healthcare problem. Despite this, osteoporosis does not get nearly as much attention as other painful problems, diseases or conditions - perhaps due to it being a “silent disease”.
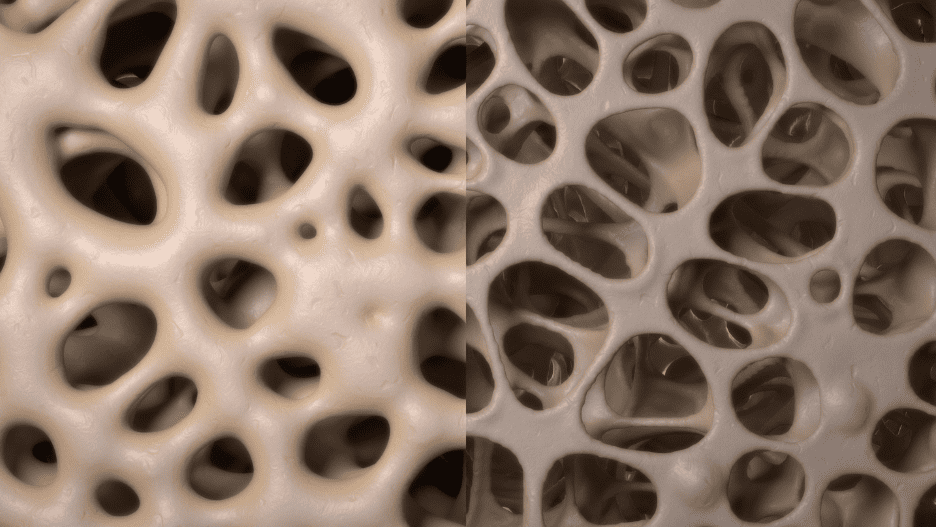 The
term osteoporosis literally translates to “bones with holes”. It is a condition that is diagnosed when your
bone mineral density, meaning how much calcium and other types of minerals are present in an area of your bone, is significantly reduced -
approximately 2.5 standard deviations or more below the average value, according to WHO criteria. Simply put, when your normally dense and
mineral-filled bones lose enough of this mineral ‘filling’ that it leaves them significantly weaker and more vulnerable to
fractures, osteoporosis is present.
The
term osteoporosis literally translates to “bones with holes”. It is a condition that is diagnosed when your
bone mineral density, meaning how much calcium and other types of minerals are present in an area of your bone, is significantly reduced -
approximately 2.5 standard deviations or more below the average value, according to WHO criteria. Simply put, when your normally dense and
mineral-filled bones lose enough of this mineral ‘filling’ that it leaves them significantly weaker and more vulnerable to
fractures, osteoporosis is present.
There is also a condition called osteopenia, often nicknamed ‘pre-osteoporosis’, which means that your bone mineral density has decreased below normal values, but is not yet low enough for you to be formally diagnosed with osteoporosis. Osteopenia is a big warning sign that osteoporosis is not far behind if your current daily activities and attention to bone health do not improve.
The symptoms of osteoporosis are often difficult to spot and recognise because they are “silent”, meaning that they occur within the bones without you knowing. For many people, they only learn that they have osteoporosis when bone density testing is performed, or if they have a fracture and the cause behind their fracture is investigated. Any ‘signs’ of osteoporosis are likely to have been manifesting over many months or years, and may include height loss, posture changes, back pain and more.
The bottom line for osteoporosis is that you cannot rely on ‘symptoms’ to spot it, and it is underdiagnosed here in Australia.
There are two types of osteoporosis:
The risk factors for osteoporosis fall into two categories: those that are modificable, and those that are non-modifiable.
Modifiable risk factors are the ones that you have at least some control in changing to be able to better improve your bone health. These are the ones that must be addressed when you are looking to prevent osteoporosis, improve your bone health, and stop a diagnosis of osteopenia from progressing to osteoporosis. They include:,
Non-modifiable risk factors are the ones you can’t control and include:
As mentioned, previous fractures are also notable risk factors. The earlier the age at fracture and the greater the number of previous fractures, the greater the subsequent risk. The risk of vertebral fractures is at least two-fold in those with previous vertebral fractures. A wrist fracture doubles the risk of hip fracture and triples the risk of vertebral fracture.
 Osteoporosis
is typically diagnosed with bone mineral density testing or DEXA scans. This is a painless test during which you lie on a table and a
scanner passes over your body to capture the data on the density of your bones.
Osteoporosis
is typically diagnosed with bone mineral density testing or DEXA scans. This is a painless test during which you lie on a table and a
scanner passes over your body to capture the data on the density of your bones.
Osteoporosis treatment is highly tailored to your unique circumstances, age and lifestyle factors. Your doctor will discuss with you when discussing the results of your bone mineral testing, but it may include taking bone-building medications like bisphosphonates or denosumab, using hormone-replacement therapy like oestrogen, or nutritional supplements like calcium and vitamin D.
From a podiatry perspective, we have been achieving fantastic results with the MLS laser. The laser is a painless and effective way to help accelerate the healing of fractures as it activates osteoblasts (bone cells) to lay down new bone at a faster rate.
We’d also like to highlight the importance of regular exercise, as weight-bearing exercise is proven to be a treatment and prevention method for both postmenopausal and age-associated osteoporosis. Incorporating various forms of physical activity into a daily routine is shown to improve muscle function and offset age-related muscle morphology changes. To best benefit from the results, the National Osteoporosis Foundation recommends skeletal loading with high and low-impact weight-bearing exercises for at least 30 minutes per day, 5–7 days a week.
Our podiatrists can also support those living with osteoporosis through the use of custom foot orthotics to help improve comfort, stability and confidence on the feet, as well as doing a footwear review to ensure the risk of falls (and hence osteoporotic fractures) is minimised.
The best way to prevent osteoporosis is to adjust your modifiable risk factors while proactively taking further actions that support your bone health. This includes ensuring your diet contains enough calcium, vitamin D and other other nutrients, avoiding smoking due to its ability to decrease oestrogen levels in women and inhibit new bone development, limit your alcohol intake, ceasing unprescribed steroid use, maintaining a healthy BMI and managing your stress levels.
Osteoporosis can run in families, likely because of inherited factors that affect bone development.
Osteoporosis is not painful in that you do not feel your bone mineral density reducing. What can be painful is an osteoporotic fracture.
It reduces your bone mineral density which makes them significantly weaker and more vulnerable to fractures and damage.
This depends on how technical you want to be, and different medical organisations hold different interpretations of this term. If ‘reversible’ implies restoring the health of a 70-year-old bone to its 30-year-old density, strength and function, then no - osteoporosis is not reversible. However, there are many things you can do to slow bone loss, improve it, and even help strengthen and rebuild bones. So if your definition of reversing osteoporosis means to improve your bone health and stop the process by which you continue to lose bone, then yes, you can achieve stronger, healthier bones, improve your quality of life, and reduce your fracture risk.
During exercise, the bones are loaded and resistance is applied to the bone. The body reacts to this by strengthening bones and muscles. It should be noted that studies have shown ‘light’ exercise to not be efficient in helping optimise bone strength, and greater loading is encouraged. This can be achieved by using a weight during walking, or even slowing down your walking pace so that the bones are exposed to the constant load from the ground for a longer period of time instead of switching from one foot to the other.
Without treatment, your bone mineral density will likely keep deteriorating, putting you at a significant risk of fractures and injury.
A bone scan identifies reductions in bone mineral density, which then meets the clinical criteria to diagnose osteoporosis when the density is reduced past a certain level.
Depending on the value of the density, you may either have osteoporosis or osteopenia (pre-osteoporosis).
In serious cases of osteoporosis, particularly in areas like the spine, the nervous system can be affected and result in numbness, tingling, or weakness. If you have notable changes in your spinal curvature related to your osteoporosis, you may also experience difficulty walking and problems with balance, which means you are at increased risk of falling and breaking other bones, such as the hips.
No it is not. Although interestingly, recent research has indicated overlapping pathways between bone biology and the biology of inflammation.
Aside from adding calcium and vitamin D into your diet, research from the Framingham Osteoporosis Study on over 5,000 adult men and women have shown that various other foods and nutrients play an important role in bone health too, including vitamin C, carotenoids, folate and B12, vitamin K, potassium, magnesium, fish (three or more servings per week), omega-3 fatty acids, dairy products (whose nutritional benefits go above calcium and vitamin D to include magnesium, zinc, riboflavin and protein), protein, and more. You can read more about this here.
| Monday | 7:40am - 6:00pm |
| Tuesday | 7:40am - 6:00pm |
| Wednesday | 7:40am - 6:00pm |
| Thursday |
7:40am - 6:00pm |
| Friday | TEMP CLOSED |
| Saturday | CLOSED |
| Sunday | CLOSED |
Ground Floor, 344 Queen Street,
Brisbane City QLD 4000
| Monday | 7:40am - 6:00pm |
| Tuesday | 7:40am - 6:00pm |
| Wednesday | 7:40am - 6:00pm |
| Thursday |
7:40am - 6:30pm |
| Friday | 7:40am - 5:00pm |
| Saturday | 7:40am - 4:30pm |
| Sunday | CLOSED |
Newmarket Village, 114/400 Newmarket Rd, Newmarket QLD 4051