Jump to section
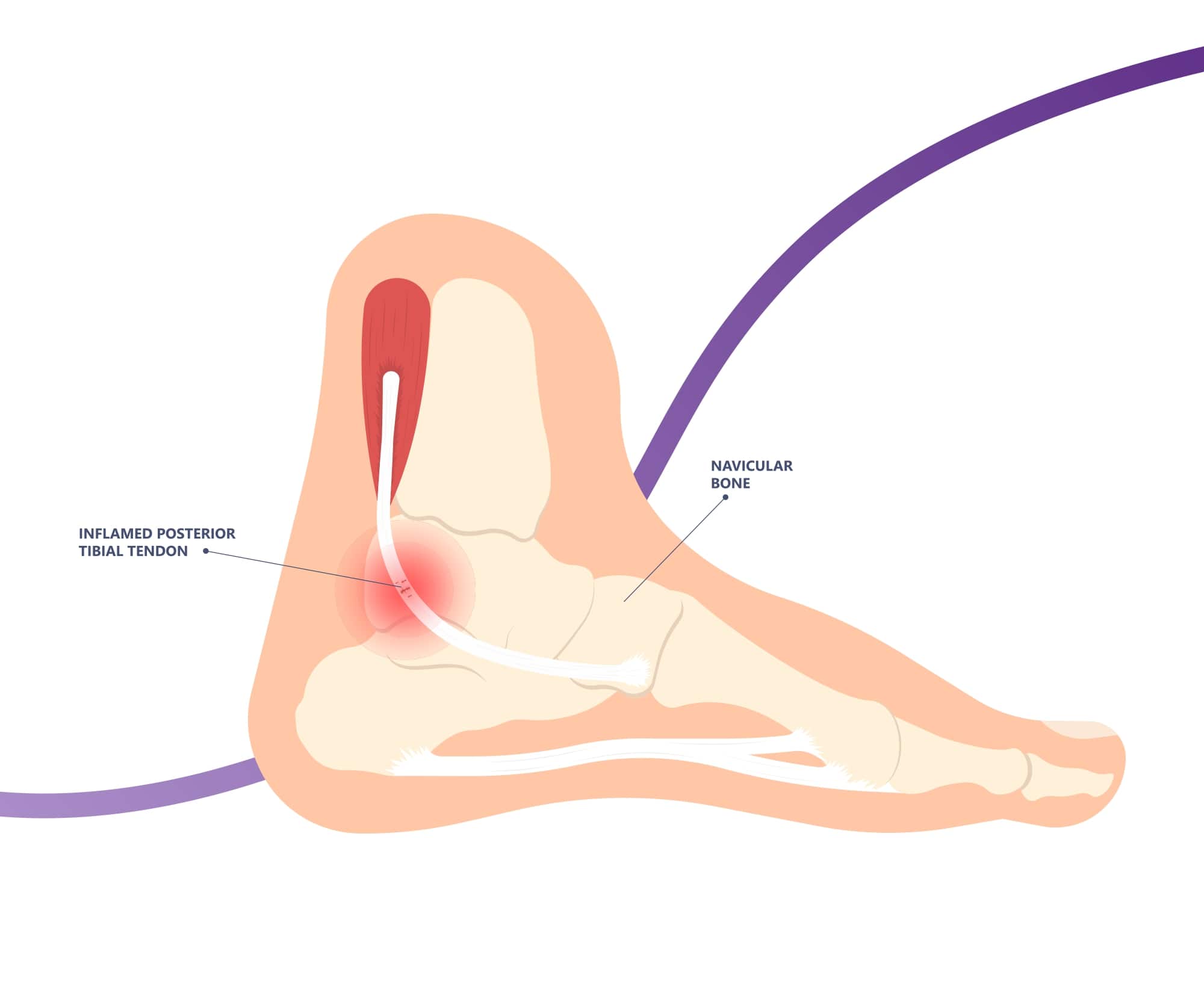
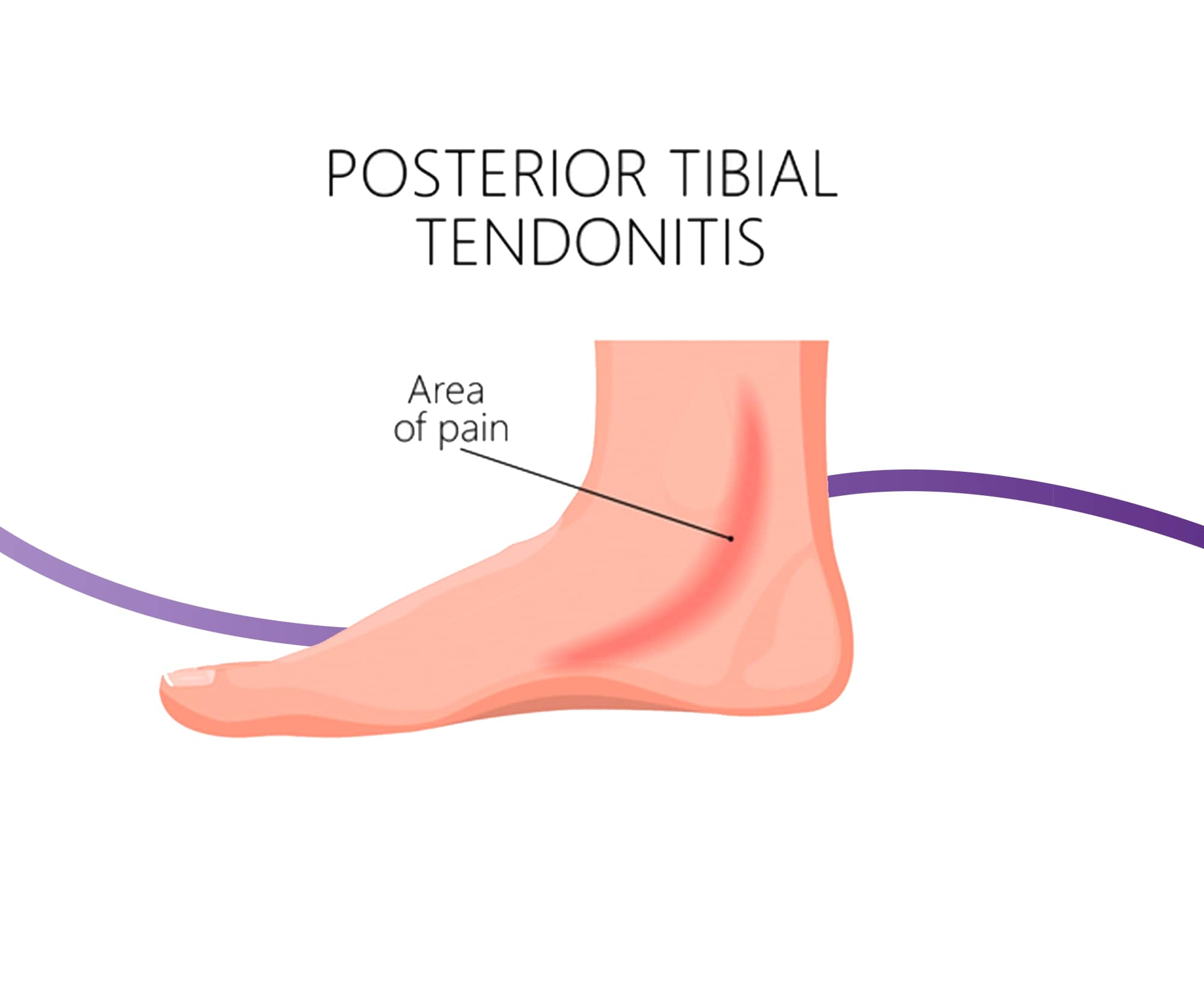
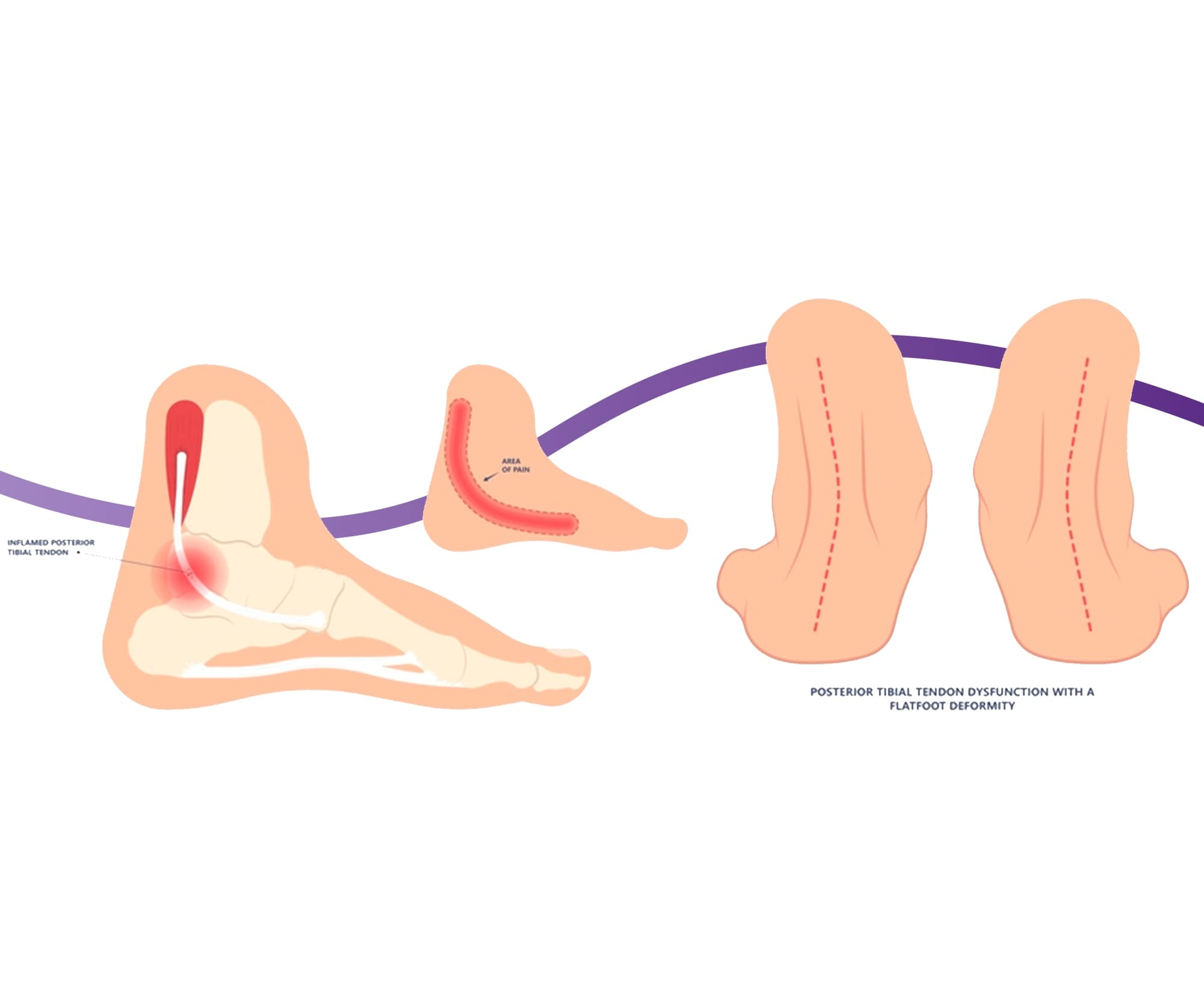
Posterior tibial tendon dysfunction (PTTD) describes the damage to a tendon called the posterior tibial tendon, which travels down the side of our lower leg, crosses the inside of our ankle, and attaches to the underside of the foot. The posterior tibial tendon plays a very important role in the structure of our foot and arch, as well as helping support healthy and pain-free movement every time we take a step.
PTTD is the most common cause of adult acquired flatfoot deformity, where the foot progressively flattens in adulthood.
There are four stages of PTTD, with each stage adding onto the former and progressing as the condition worsens:
Stage I
Stage one of PTTD carries little or no symptoms, with ultrasound and other imaging studies showing a relatively normal result, aside from some mild inflammation of the tissue surrounding the tendon. The discomfort associated with this inflammation is often the first sign for many, but it is often ignored as something presumed to be short-lived that will resolve on its own.
At stage one, you can also successfully complete a single heel raise. To perform the raise, hold onto the wall or the back of a chair with one hand. Stand up straight and lift the unaffected foot up off the ground. Now, attempt to lift onto the toes of the affected foot. You should be able to complete this, though some minor discomfort may be noted.
Stage IIA
At stage two A, your foot will have flattened somewhat as the posterior tibial tendon is no longer functioning well enough to support the arch, which will be confirmed on imaging studies. You will no longer be able to perform a single leg heel raise, meaning you can no longer lift up on the toes of the affected leg due to the pain. You may also experience some pain in your sinus tarsi on the outside of the ankle. Your rearfoot will be flexible, and the forefoot will still be relatively normal.
Stage IIB
Stage two B includes all of the features of stage two A, but the forefoot will now be
in abduction, meaning that the front of the foot is facing out away from the midline of the body. As a result, when looking
from the back of the heels, you may notice more toes being visible on the outside of the foot.
Stage three
This stage of PTTD is when the changes at the foot and ankle become
inflexible or rigid. Adding onto stage two, imaging studies may also reveal arthritis at the ankle joint, alongside the arch
collapse.
Stage
four
Stage four is the final and worst stage. The joints have significantly deteriorated and become arthritic. The arch has completely
collapsed and the foot has become rigid and painful on the outer ankle.
These stages come into play clinically when we look at treatment - it is much simpler to treat stage one and two PTTD and set the tendon up
for healing, whereas at stages three and four substantial and often irreversible damage has occurred, so it’s about making you as
comfortable as possible in everyday life.
As PTTD progresses through the stages, the symptoms worsen as the arch collapses and the foot grows to become rigid and fixed in place. In
the early stages of PTTD, you may notice:
PTTD is an overuse condition, meaning that it is caused by repetitive overloading of the tendon past what it can safely handle, which leads to microtrauma and progressive failure of the tendon so it can no longer carry out its role sufficiently.
Contributing factors to the development of PTTD can include:,
Diagnosing PTTD starts with an assessment with your podiatrist that serves to assess your feet and legs, rule out other pathologies that can produce similar symptoms, and confirm your PTTD diagnosis. PTTD can be diagnosed without any medical imaging, though it can be helpful to understand the severity of the damage and accurately grade the PTTD according to its stage, which then influences the best treatment approach. Conditions we want to rule out during your assessment include:
Your comprehensive assessment with us includes:
Just because you have recently started experiencing pain at the posterior tibial tendon, or are in the early stages of the condition, does not mean that you are destined to progress to the debilitating later changes. By working with a podiatrist and implementing a personalised treatment plan, you can help repair the damage, and prevent it from progressing any further - ultimately leaving it as the same strong and healthy tendon it was previously.
The best approach to managing PTTD varies greatly depending on the stage of severity. It is important to emphasise that it is significantly simpler for you to treat stage one and two PTTD and set the tendon up for healing, compared to stages three and four where substantial and often irreversible damage has occurred.
Your podiatrist will explain everything to you, including all of the options that are relevant and appropriate for your current symptoms.
Non-surgical treatment forms the basis of all of our treatment plans for PTTD with our podiatrists, given that surgery is a serious and invasive procedure that carries its own risks and complications. We may recommend:
Activity modification, ice and the use of non-steroidal anti-inflammatory medication (NSAIDs) are all a first-step conservative management approach that you can use immediately, before your appointment with your podiatrist, to help relieve some discomfort associated with PTTD. While these are not a treatment to repair the problem, they can help temporarily improve comfort, mobility and quality of life.
Custom foot orthotics work by reducing the strain on the already-damaged posterior tibial tendon with every step you take. The orthotics we create are designed completely for your feet after a comprehensive assessment and 3D foot scan. Instead of your foot rolling down which would stretch and strain the damaged tendon, one of the many ways your orthotics work is by supporting your arch and tendon so it gets a chance to heal.
Bracing
Braces are an effective way to help feet affected by PTTD by supporting the leg, foot and arch in an optimal position. This position is one where the posterior tibial tendon is not strained through every step, and so has a chance to repair, instead of continuing to be overused and risk progressing through the stages. Braces also help to restrict painful motion, compensate for lost motion, accommodate deformity, provide support, and subsequently improve gait and ambulation.
We’re proud to offer a range of braces for PTTD, including:
We also offer customised bracing with an in-built custom orthotic, as well custom-made footwear where we work together with a pedorthist. The best option for you will be discussed with your podiatrist on a case-by-case basis.
Where there is significant damage to the posterior tibial tendon, immobilisation with a walking boot for up to 3-4 weeks may be used to create an optimum environment for the damaged tendon to heal.
Using eccentric strengthening exercises, taught to you by our podiatrists, can help to regain strength and function when implemented at appropriate times. We also examine the strength and flexibility of the entire foot and ankle and include these aspects in your stretching and strengthening program.
We pair your custom foot orthotics with good, supportive footwear that best helps to control the movement at the foot and ankle, and reduce the strain on the posterior tibial tendon.
While surgery is not a first-line treatment for us, if your PTTD has reached stage three or four where you have arthritic changes and notable deformities, or you have had pain for over 6 months and conservative methods have failed, it should be considered along with your other treatment options. In this case we can refer you to an orthopaedic surgeon for a consultation so you know all of your options.

Our feet are the foundation for the entire body, so it's important that they have enough strength to tolerate our activity levels. Use
these three exercises to help strengthen your feet.

Not everyone needs orthotics, but they can play an integral role in treating or relieving pain in several foot and lower limb conditions.

The heat and humidity of an Australian summer makes it a prime time for issues to arise, so our newest podiatrist Lucy has put together
seven helpful tips to keep your feet healthy and problem free throughout summer.
| Monday | 7:40am - 6:00pm |
| Tuesday | 7:40am - 6:00pm |
| Wednesday | 7:40am - 6:00pm |
| Thursday |
7:40am - 6:00pm |
| Friday | TEMP CLOSED |
| Saturday | CLOSED |
| Sunday | CLOSED |
Ground Floor, 344 Queen Street,
Brisbane City QLD 4000
| Monday | 7:40am - 6:00pm |
| Tuesday | 7:40am - 6:00pm |
| Wednesday | 7:40am - 6:00pm |
| Thursday |
7:40am - 6:30pm |
| Friday | 7:40am - 5:00pm |
| Saturday | 7:40am - 4:30pm |
| Sunday | CLOSED |
Newmarket Village, 114/400 Newmarket Rd, Newmarket QLD 4051