Jump to section
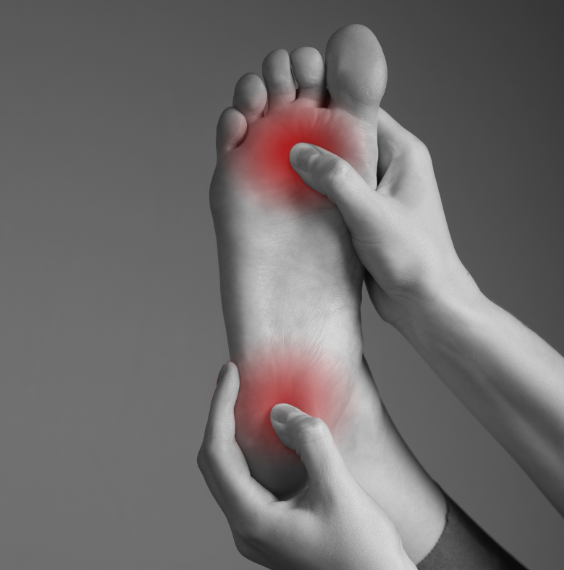
Fat pad atrophy occurs when the fat pads on the bottom of the foot thin and become less effective at protecting the bones beneath,
increasing our likelihood of foot pain and injury.
We have cushion-like fat pads at the bottom of our heels, as well as the balls of our feet, that are designed to help protect the underlying bones and tissues. They absorb shock and ease the large load placed on our feet on a daily basis. Unfortunately, over time, this protective layer of fat can break down and become thin, or displace forwards, leaving the underlying bones and joints more vulnerable to pressure-related discomfort and pain.
The natural ageing process is the most common cause for this gradual fat pad thinning, occurring as the fat content within the pad reduces and structural changes within the connective tissues occur. This diminishes the effectiveness of the fat pad as a shock absorber. Other causes or contributing factors include:
While symptom severity will vary from person to person, thinner fat pads will make our bones more prominent and vulnerable to damage, particularly at our metatarsal heads (at the ball of the foot) and at the heel. As such, most symptoms will occur in these two areas and can include:
Your podiatrist can confidently diagnose fat pad atrophy with a clinical exam that involves palpating the heels and soles of your feet to check for prominent bones and damage, as well as getting to know your medical history. If your podiatrist suspects that as a result of your fat pad atrophy there has been damage to the bones or structures in the heel or forefoot, then imaging may be used to better understand the nature of these injuries. Our podiatrists are also able to use pressure mapping to understand how weight is being distributed across your feet and where bony prominences may be putting you at risk of pain and injury.
There are several conditions that may present with similar symptoms to fat pad atrophy, which is why it’s important to work with an experienced podiatry team that will investigate thoroughly to rule out the alternative causes for your foot pain. These involve plantar fasciitis that produces pain at the bottom of the heel, metatarsalgia, arthritis, tarsal tunnel syndrome and more.
The fat cells in your feet can’t regenerate once the fat pad has broken down, so the goal of your treatment is to both substitute the ‘cushioning’ your feet are now lacking in other ways, while ensuring that the rate of any further fat pad atrophy is not accelerated. Our podiatrists achieve this by:
While we can’t prevent the natural effects of ageing, we may be able to slow the start and progression of fat pad atrophy by maintaining a healthy weight, choosing supportive footwear with proper cushioning, and opting for lower impact exercises as opposed to high-intensity repetitive movements.
As most of the uncomfortable symptoms of fat pad atrophy are associated with having insufficient cushioning in the area, as soon as we are able to provide that using a combination of footwear or orthotics, you should notice an immediate difference. If you have any conditions alongside the atrophy, such as joint inflammation, then it may take several weeks (if not longer) to allow that to heal and return to a minimally painful state.
You can start getting some relief before you can make it in to see your podiatrist by applying ice packs to the feet, elevating the feet, and using over-the-counter anti-inflammatory medications. Wear shoes with adequate cushioning both inside and outside of the home.
| Monday | 7:40am - 6:00pm |
| Tuesday | 7:40am - 6:00pm |
| Wednesday | 7:40am - 6:00pm |
| Thursday |
7:40am - 6:00pm |
| Friday | TEMP CLOSED |
| Saturday | CLOSED |
| Sunday | CLOSED |
Ground Floor, 344 Queen Street,
Brisbane City QLD 4000
| Monday | 7:40am - 6:00pm |
| Tuesday | 7:40am - 6:00pm |
| Wednesday | 7:40am - 6:00pm |
| Thursday |
7:40am - 6:30pm |
| Friday | 7:40am - 5:00pm |
| Saturday | 7:40am - 4:30pm |
| Sunday | CLOSED |
Newmarket Village, 114/400 Newmarket Rd, Newmarket QLD 4051