Jump to section
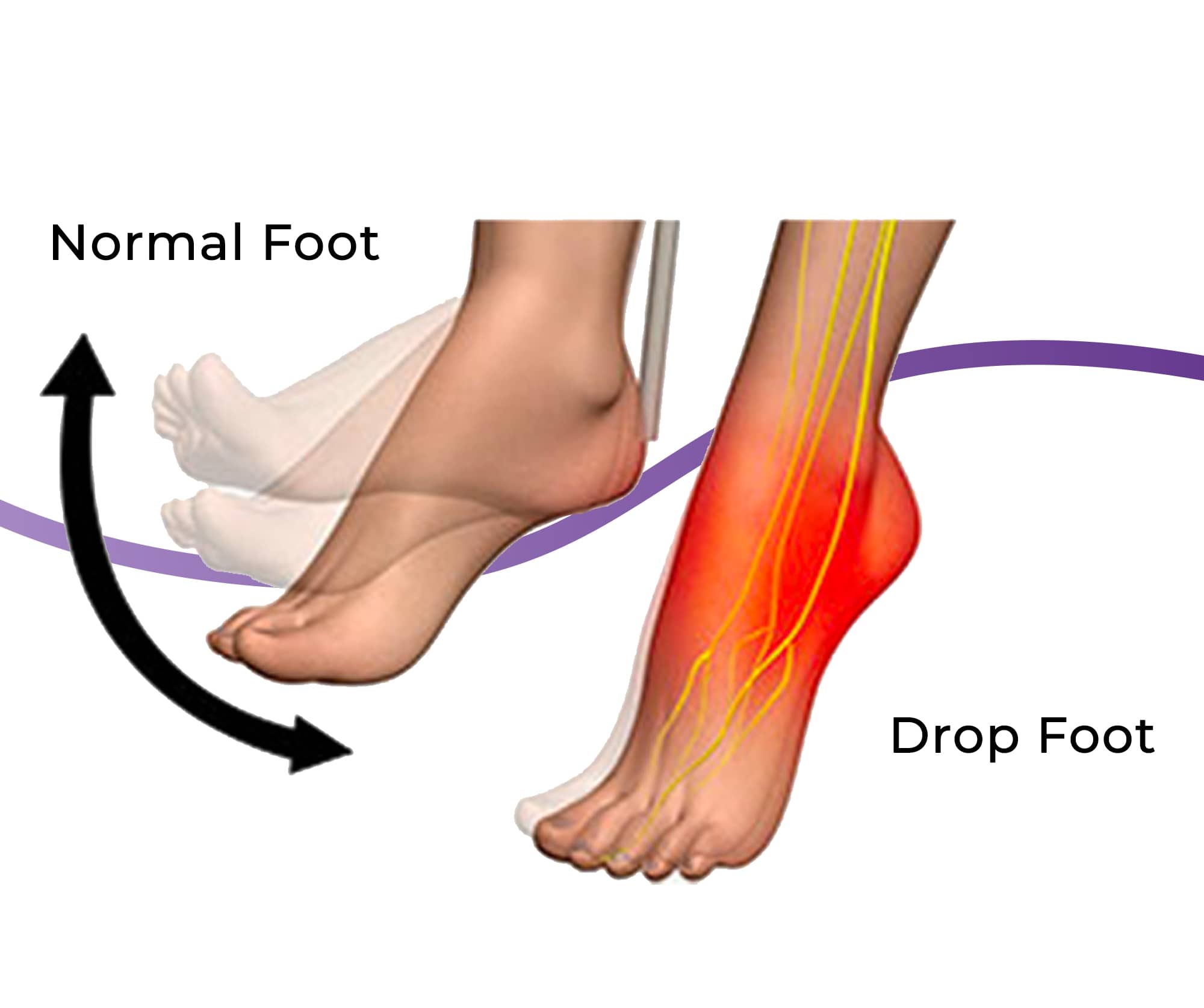
When you have a dropped foot, or foot drop, it means that weakness in one or both of your legs makes you either unable to move your ankle to point your toes up towards the sky, or you have great difficulty doing so. When this happens, your foot remains in a dropped position when you walk, with your toes hanging downwards. This makes it difficult for your foot to clear the ground as you walk, putting you at risk of tripping and falling from your toes hitting the ground - or forcing you to compensate for the foot drop by excessively lifting and bending your knee and hip - which can cause a new series of problems over time and increase the likelihood of a fall with 1 in 3 Australians over the age of 65 being hospitalised from a fall each year. Majority of falls are preventable.
If you have foot drop, you’ll feel a noticeable weakness when moving your foot up and around on your ankle, with your foot having a heavy feeling. You may experience some tingling or numbness in your foot, curling toes, and may notice that your foot drags along the ground or catches the ground during regular walking - if you don’t lift your knee higher than normal to stop it from touching the ground.
***please insert image of peroneal nerve***
Foot drop is really a symptom of an underlying problem with one of your nerves called the peroneal nerve, which is responsible for innervating the muscles that work to seamlessly lift your foot up relative to your ankle. While one of the most common causes of damage to the peroneal nerve we see is through trauma or an accident, like during a sudden knee dislocation, direct impact to the nerve during a fall or during sports, or a fracture to the fibula, there are many other issues that can also affect the peroneal nerve, including:
While it may seem clear if your foot is dragging and dropping down, it’s important to take a full history, assess the function of your peroneal nerve and look at what has likely caused the nerve damage, so that the best course of action for treatment and management can be recommended.
Your physical examination will assess the status and function of the common peroneal nerve (meaning the main branch of the peroneal nerve), and then look beyond the nerve for any other signs and symptoms that can indicate what is causing the problem, such as:
Your physical examination will also involve muscle strength testing, range of motion testing, a video gait analysis, in-shoe pressure assessment, a foot posture index and more.
Your podiatrist may also use the Tinel sign test to help pinpoint the area of nerve irritation or entrapment by tapping along the course of the nerve, particularly around the neck of the fibula bone. If tingling or numbness is felt along the area that is tapped, it is a positive Tinel sign.
Medical imaging such as x-rays, ultrasounds and CT scans may be used to examine for damage to the fibula bone (as the peroneal nerve is located close to the fibula neck), the position of soft tissues that may have entrapped or compressed the nerve, exclude soft tissue masses, and more.
Nerve tests, such as the nerve conduction velocity (NCV) tests and electromyography tests (EMG), can help give a greater insight into the motor and sensory fibres of the peroneal nerve and its deep and superficial branches, helping understand the cause of the foot drop. Nerve tests can also help to pinpoint where along the nerve the injury has occurred.
Being diagnosed with foot drop can be done from a physical examination with our podiatrists, who can also refer you for imaging studies as needed. We do not perform nerve studies, however, so if the cause of your foot drop is unclear and further testing is needed, we can refer you to a nerve specialist.
Managing foot drop is very different from managing muscle, tendon or joint injuries because nerve damage can often be unpredictable. Some cases of foot drop may resolve in weeks or months, while others may be longstanding or permanent. It can vary greatly depending on the way the nerve was injured and the severity of the injury.
Here at The Feet People, our Brisbane podiatrists work extensively with patients with foot drop to help get them back to moving comfortably while reducing any further injury risk that may come from tripping over the toes and falling. Our goal is to:
We’re proud to offer Brisbane’s leading brace for foot drop - the EXO-UP brace. This brace is unique in that it is 100% customised for your lower leg - it is 3D scanned and then custom made to fit your foot and your shoe perfectly. There is no guesswork or discomfort arising from an ‘almost’ right fit. The brace works together with your shoe, holding your toes up with every step.
What our patients love most about this brace is that it is small and discreet - far from any of the bulky, obvious and clunky braces available on the market. Read more about the EXO-UP brace here.
We also offer other alternatives to the EXO-UP including ankle-foot orthoses, which encompass the foot, ankle and lower leg. Your podiatrist will discuss all of your options with you alongside the factors that you need to consider, such as:
Physical therapy for foot drop includes a program of stretching, strengthening, mobilisation, manipulation, and proprioceptive and
balancing exercises. This is something our podiatrists can help you with, with your physical therapy plan adjusting as you progress and
regain strength and movement in your foot.
Nerve stimulation uses functional electrical stimulators (FES) to help enhance movement or function of the muscles and the lower limbs
by applying electrical currents to the peripheral nerves. If you are not experiencing the progress we’d expect, we are able to
refer you to a nerve specialist to look into whether this treatment could be right for you.
Surgery is not a first-line treatment for foot drop, however, it can be explored in cases such as the presence of a rapidly deteriorating lesion, no signs of improvement within three months, and open injuries with a suspected nerve laceration.
In most cases, nerve damage occurs as a result of a sudden and unexpected injury, and therefore cannot be prevented. Where nerve damage is a
result of diabetes, best managing a person’s diabetes can reduce its rate of progression of the damage.

Our feet are the foundation for the entire body, so it's important that they have enough strength to tolerate our activity levels. Use
these three exercises to help strengthen your feet.

Not everyone needs orthotics, but they can play an integral role in treating or relieving pain in several foot and lower limb conditions.

The heat and humidity of an Australian summer makes it a prime time for issues to arise, so our newest podiatrist Lucy has put together
seven helpful tips to keep your feet healthy and problem free throughout summer.
| Monday | 7:40am - 6:00pm |
| Tuesday | 7:40am - 6:00pm |
| Wednesday | 7:40am - 6:00pm |
| Thursday |
7:40am - 6:00pm |
| Friday | TEMP CLOSED |
| Saturday | CLOSED |
| Sunday | CLOSED |
Ground Floor, 344 Queen Street,
Brisbane City QLD 4000
| Monday | 7:40am - 6:00pm |
| Tuesday | 7:40am - 6:00pm |
| Wednesday | 7:40am - 6:00pm |
| Thursday |
7:40am - 6:30pm |
| Friday | 7:40am - 5:00pm |
| Saturday | 7:40am - 4:30pm |
| Sunday | CLOSED |
Newmarket Village, 114/400 Newmarket Rd, Newmarket QLD 4051