
Jump to section
It is very common for our podiatrists to hear that when a person develops heel pain, they quickly
suspect that their pain is caused by a heel spur. While ‘heel spurs’ have become a common term to explain heel pain, this
isn’t technically accurate, and for over 95% of the patients we see with pain at the bottom of their heel, the true cause of pain
is actually a condition called plantar fasciitis.
Interestingly, heel spurs are present in about 15% of the general population, many of whom won’t ever know they have one, unless it is coincidentally discovered on an x-ray while investigating something else. Of those with heel spurs, less than 5% actually have heel pain. To help solve the confusion, here’s a look into what heel spurs really are, and why they occur.
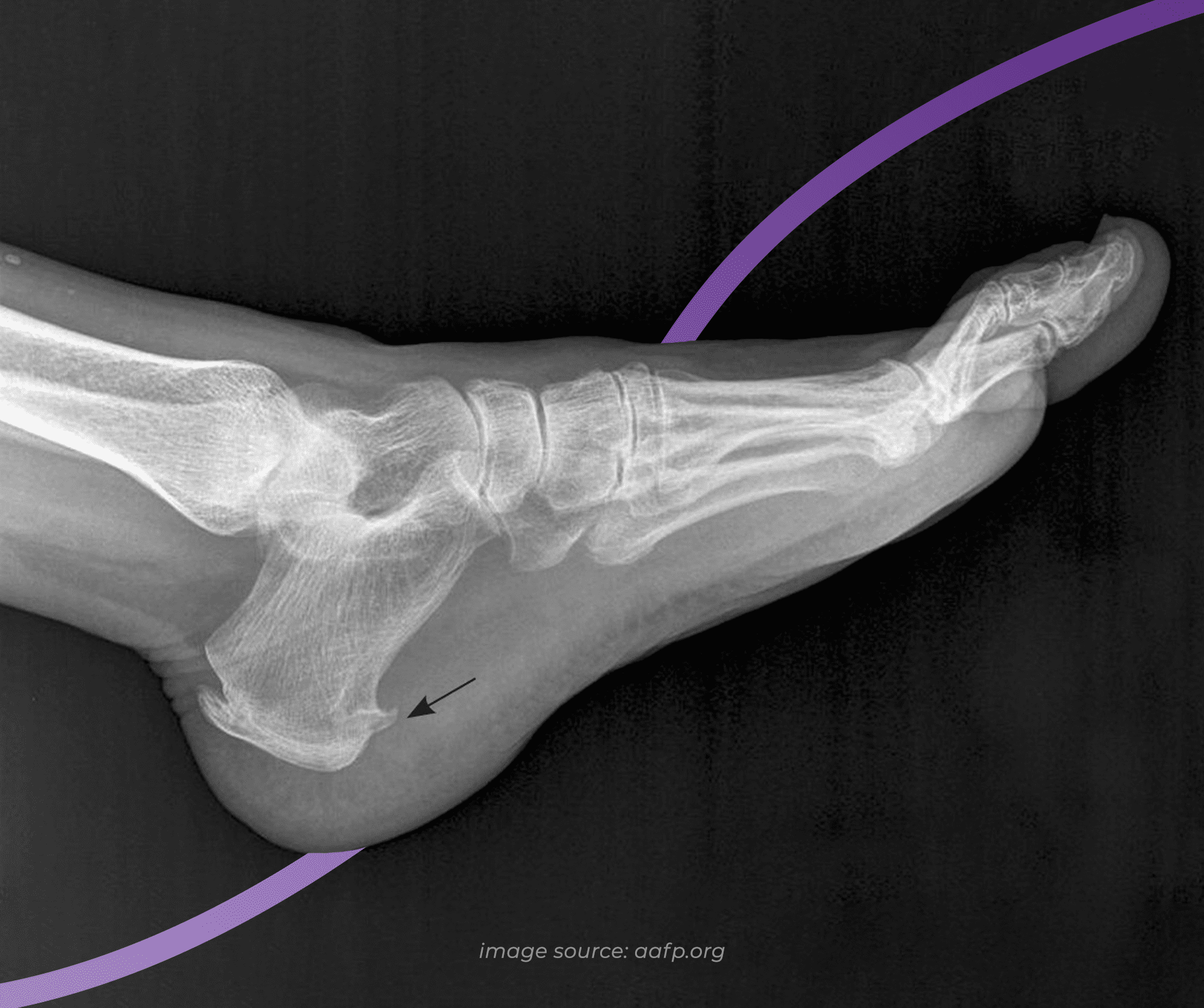
A heel spur, otherwise known as an osteophyte, is a bony outgrowth that starts at the heel bone. Looking at an x-ray, the spur often looks like a small spike or hook which faces the inside of the arch - an appearance that leaves many automatically assuming that they must be like a painful splinter. What an x-ray doesn’t show is that the spur sits in line with the tissue fibres that it is embedded in, as opposed to piercing them, which is why most people don’t notice their heel spur.
A heel spur is made of calcium deposits that build gradually over many months or years. While here we’re using the example of a spur
at the bottom of the heel that is often mistaken for plantar fasciitis, spurs can develop anywhere that tendons attach to bone - whether
that be at the back of the heel bone at the Achilles tendon, or on other bones across the the body.
The symptoms of a heel spur can be tricky to describe because most heel spurs are asymptomatic, and most times when patients come to us looking for answers to their heel spur pain, they are actually looking for answers to their plantar fasciitis pain, but have confused the term due to the way it is commonly used.
When heel spurs are symptomatic, they can aggravate the tissue that they’re associated with, which in this case is the plantar fascia, producing symptoms including:
Heel spurs have been shown to develop in response to damage and strain to the soft tissues that insert at the bottom of the heel - in this case, the insertional fibres of the plantar fascia tissue. When the plantar fascia, which connects to the bottom of the heel bone, repetitively pulls on and places stress on the heel during movement, this creates micro-trauma. The body responds by trying to repair the area by creating more bone - this becomes the calcified protrusions that we know as heel spurs.
Anything that exacerbates the pulling and stress on the heel bone from the plantar fascia will contribute to the development of a heel spur, including:
Heel spurs may also be caused by inflammatory arthritis, and may be encouraged by other problems like the breakdown of the fat pad of the heel.
Having plantar fasciitis (or any tendinopathy elsewhere in the body) that has been present for over 8 weeks places you at a higher risk of developing heel spurs, as it demonstrates that there is excess tension and pulling at the tissues with the body trying to repair the condition. This places certain groups of people at a higher risk of heel spurs:
Due to the similarity in symptoms between a heel spur and other causes of heel pain like plantar fasciitis, confidently diagnosing a heel spur specifically includes taking your medical and injury history, a comprehensive clinical exam, and an x-ray.
Even when a heel spur is confirmed via x-ray, it can be difficult to confirm if your pain is actually related to the spur, or if it is coincidentally present while it is your plantar fascia tissue that is producing the pain. Thankfully, the initial treatment for both plantar fasciitis and a heel spur is the same, and the assessments performed by our podiatrists are always comprehensive and designed to give you the most information and answers to why your pain has developed.
Treating a spur at the bottom of your heel follows the same treatment plan as plantar fasciitis, because of the unique way in which the two are connected. This may include:
For almost all of our patients that have heel spurs confirmed with an x-ray, following our proven treatment methods completely resolves all of the painful symptoms, meaning that the heel spur will not require direct treatment with surgery or other methods. If conservative treatment methods fail, however, surgery may be considered as a last resort.
If you ignore heel pain, then there is a good chance that your pain will persist and may even worsen to limit what you can do on a daily basis, which is why we always recommend promptly treating any heel pain that develops. If your heel spur is detected accidentally without any pain or symptoms, however, or if treating plantar fasciitis resolves your symptoms, then treatment is not indicated for the spur itself, and it is fine to ignore. In these cases, it is likely that the spur may remain and not cause you any problems.
It is not clear why heel spurs develop in some people with tissue stress on their heel bone and not others, but the best way to help prevent heel spurs developing is to treat any heel pain that arises promptly, without allowing significant stress to continue for prolonged periods. This is where working with your podiatrist for your heel pain is key. As podiatrists are foot health experts, by working with your podiatrist, you can expect:

If you are injured and experiencing heel pain, the first thing you should do is look at your activity levels and modify them if needed.
Follow these three simple rules to help manage your heel pain

Not everyone needs orthotics, but they can play an integral role in treating or relieving pain in several foot and lower limb conditions.

The heat and humidity of an Australian summer makes it a prime time for issues to arise, so our newest podiatrist Lucy has put together
seven helpful tips to keep your feet healthy and problem free throughout summer.
| Monday | 7:40am - 6:00pm |
| Tuesday | 7:40am - 6:00pm |
| Wednesday | 7:40am - 6:00pm |
| Thursday |
7:40am - 6:00pm |
| Friday | TEMP CLOSED |
| Saturday | CLOSED |
| Sunday | CLOSED |
Ground Floor, 344 Queen Street,
Brisbane City QLD 4000
| Monday | 7:40am - 6:00pm |
| Tuesday | 7:40am - 6:00pm |
| Wednesday | 7:40am - 6:00pm |
| Thursday |
7:40am - 6:30pm |
| Friday | 7:40am - 5:00pm |
| Saturday | 7:40am - 4:30pm |
| Sunday | CLOSED |
Newmarket Village, 114/400 Newmarket Rd, Newmarket QLD 4051